The Gut-Brain Axis
Improving Mental Health Through Digestive health
Now more than ever, digestive health is a promising area of exploration for the advancement of medical research and enhancement of quality of life.
Have you ever been told “you are what you eat”? Well, recent studies have demonstrated validity in this common saying. There is a definable relationship between the gut’s microbiome and mental health. This relationship is known as the Gut-Brain Axis (1). Many systems of the body communicate in ways which extend beyond our cognitive scope in daily life, but the Gut-Brain Axis is a unique example of this phenomena as this relationship directly influences our mood and mental processing.
90% – 95% of the body’s Serotonin is produced in the gut (2). Serotonin, known as the “happy chemical”, is a neurotransmitter which regulates central nervous system functions such as reward systems, happiness and mood, cognitive processes, sleep and appetite, as well as learning and memory (3). In the nervous system, neurotransmitters act as messengers which relay information to and from nerve cells.
Increased serotonin production is widely sought out as a method of treating ailments in the fields of pharmacology, psychiatry, psychology, and neurology. Whether it be through medication, such as antidepressants, or environmental changes for increased serotonin production / reuptake, such as exposure to sunlight, serotonin receptors are often directly or indirectly targeted for improved wellbeing. This is because a lack of adequate amounts of serotonin can potentially result in challenging mental health conditions. Some neurotransmitters, including Serotonin, have been recently found to fulfill their roles outside of the nervous system.
In the gut, billions of bacteria coexist to assist in the breakdown of food, maintain the health of working cells, and protect intestinal lining. An important type of cell supported by the gut’s bacteria is the Enterochromaffin cell. These cells are greatly responsible for the secretion of serotonin. Studies that examine the relationship between mental health or quality of life and the amount of healthy gut bacteria show hopeful results (4), making it seem that Enterochromaffin cells nearly depend on healthy gut bacteria to produce an adequate amount of serotonin. Studies that have examined the relationship between the amount of healthy gut bacteria and symptoms of depression demonstrate that individuals with Major Depressive Disorder were less likely to have an adequate amount of healthy gut bacteria(5,6).
A lack of healthy gut bacteria can also contribute to irritable bowel syndrome, fatigue, heightened sensitivity to pain, and anxiety. Unfortunately, many modern lifestyles inhibit the growth of healthy gut bacteria. Environmental toxins, stress, fast food, processed meats and sugars, antibiotic medications, and alcoholic beverages may all contribute to this issue.
With this information in mind, how do we mitigate the effects of the modern lifestyle in regard to digestive health? Maintaining a healthy gut begins with what we intake. Eating fiber rich foods, fermented foods, a variety of greens, and supplementing with probiotics is a great place to start. Probiotics are comprised of diverse types of healthy bacteria which promote the growth of other healthy bacteria in the gut.
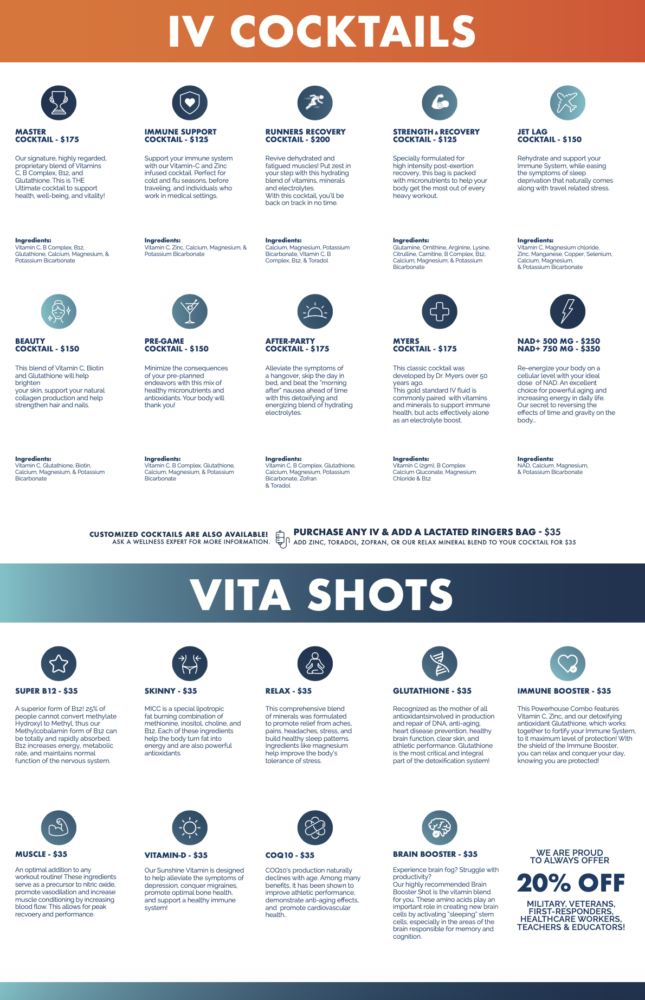
This is why the IV Lounge & Wellness Center team is proud to carry a comprehensive Digestive & Probiotic Supplement which can be taken at meal time to aid in the digestive process. It is our belief that wellness begins from within, and often times there are accessible means for improving our health, including mental health, in daily life.
References
- Carabotti, Marilia et al. “The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems.” Annals of gastroenterology vol. 28,2 (2015): 203-209.
- Terry, Natalie, and Kara Gross Margolis. “Serotonergic Mechanisms Regulating the GI Tract: Experimental Evidence and Therapeutic Relevance.” Handbook of experimental pharmacology vol. 239 (2017): 319-342. doi:10.1007/164_2016_103
- Berger, Miles et al. “The expanded biology of serotonin.” Annual review of medicine vol. 60 (2009): 355-66. doi:10.1146/annurev.med.60.042307.110802
- Appleton, Jeremy. “The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health.” Integrative medicine (Encinitas, Calif.) vol. 17,4 (2018): 28-32.
- Aizawa, Emiko et al. “Possible association of Bifidobacterium and Lactobacillus in the gut microbiota of patients with major depressive disorder.” Journal of affective disorders vol. 202 (2016): 254-7. doi:10.1016/j.jad.2016.05.038
- Limbana, Therese et al. “Gut Microbiome and Depression: How Microbes Affect the Way We Think.” Cureus vol. 12,8 e9966. 23 Aug. 2020, doi:10.7759/cureus.9966